Fue Hair Transplant Turkey
The FUE method (follicular unit extraction) is a meticulous procedure in which single hair is extracted and replanted in designated area. Hair follicles are obtained from the donor area and implanted in the bald area. FUE hair transplant does not leave a visible trace.
Fue Hair Transplant Package
The average cost of FUE Hair Transplant in Turkey is 1800 Euro. The maximum charge for Fue Hair Transplant in Turkey is up to 2200 Euro. The cost for 2025 inclusive package airport pick-up, local transfers, hotel accommodations, interpreter services, unlimited hair transplant procedure, as well as shampoo and lotions. All our operations take place in Nişantaşı, Istanbul.
| Level of Baldness | No. of Grafts Required | Average Cost of FUE Transplant |
|---|---|---|
| Level 1 | 800-1400 | 1500 Euro |
| Level 2 | 2000-2500 | 1800 Euro |
| Level 3 | 3500-4000 | 2000 Euro |
| Level 4 | Over 4000 grafts | 2200 Euro |
Procedure – Aftercare
| Country and City | Turkey – istanbul |
| Duration | 5 – 7 Hour |
| Anesthesia | Local |
| Duration of stay in Istanbul | 4 Days |
| Persistence of Results | Permanent |
| Pain and Discomfort | Partially |
| Returning to Work | 4 Days |
| First Bath | 3 Days |
| Full Recovery | 6 Month |
| Side effects | Swelling and redness |
| Exercise – Cardio | 30 Days |
| Will there be any scar? | Almost Invisible |
Fue Hair Transplant Timeline
Airport Pickup
Welcoming our patients and placing them in their hotel. Zty Health is contracted with Cityloft Hotels.
Operation Day
Hotel / Hospital Transfer. Medical examination. Health and blood tests. Hair Transplant operation.
Washing
First hair wash. Removal of stitches. Next hair wash tutorial.
Return
Hotel / Airport Transfer by VIP vehicle
Comparative Analysis of FUE Techniques
| Feature/Parameter | Standard FUE | Sapphire FUE | DHI (Direct Hair Implantation) |
|---|---|---|---|
| Incision Instrument | Steel Slit/Blade | Sapphire Blade | Choi Implanter Pen (simultaneous incision and implantation) |
| Recovery Speed | Standard (7-10 days) | Accelerated (5-7 days) | Standard (7-14 days, density-dependent) |
| Maximum Density | Good | Very Good (Enables creation of higher-density incisions) | Excellent (Facilitates implantation between existing terminal hairs) |
| Shaving Requirement | Full or partial shaving of the recipient area is generally required. | Full or partial shaving of the recipient area is generally required. | Most suitable technique for an “unshaven” or “no-shave” procedure. |
| Advantages | Cost-effective; suitable for treating large areas of alopecia. | Reduced crusting (scab formation), faster wound healing, potential for achieving higher graft density. | Precise control over the angle and direction of implantation, minimized graft out-of-body time, unshaven option. |
| Disadvantages | Higher potential for tissue trauma, comparatively slower healing. | Higher cost; the outcome is highly dependent on the surgeon’s experience. | Longer operative duration, higher cost, requires a highly experienced surgical team. |
| Ideal Candidates | Patients with extensive androgenetic alopecia and budgetary considerations. | Patients seeking to achieve maximum density and a highly defined, natural hairline. | Patients who wish to avoid shaving, require densification in specific zones, or are undergoing eyebrow/beard transplantation. |
Reviews
Visit our Google business account for all patient reviews.
What is micro fue Turkey ?
Micro FUE (Follicular Unit Extraction) is a modern technique used in hair transplantation procedures. The term “micro” in Micro FUE is often used to refer to the use of very small (micro) punches (tools) to harvest individual follicular units from the donor area. The sizes of these punches can range from 0.6mm to 1.0mm in diameter, depending on the surgeon’s preference, patient’s hair characteristics, and other factors.
In a FUE hair transplant in Turkey, individual follicular units (natural groupings of 1-4 hairs) are extracted directly from the patient’s donor area (typically the back and sides of the scalp), and then implanted into the bald or thinning areas of the patient’s scalp. Because of its minimally invasive nature, FUE generally has less post-operative discomfort and quicker recovery time compared to older, traditional methods of hair transplantation.
Micro fue Turkey hair transplant improves upon traditional FUE by further minimizing the scarring in the donor area due to the use of smaller punches. This can result in an even more natural look and less detectability of the procedure. However, the success and outcome of the procedure still largely depend on the skill and experience of the surgeon performing the procedure.
What is an FUE hair transplant?
An FUE hair transplant, or Follicular Unit Extraction, is a modern hair restoration technique. Here’s a simple explanation:
In this procedure, individual hair follicles are removed one by one from a part of your body, usually the back of the head, where the hair is more resistant to balding. Then, these follicles are planted in the areas where you are losing hair. It’s a less invasive method, which means there is no scar left behind, and the recovery time is shorter compared to other methods. Plus, it gives a more natural-looking result. It’s good to note that it might take a few sessions to get the full effect, and it can be a bit costly. It’s a popular choice because it tends to result in a very natural look and has a higher success rate. Before choosing this method, it’s best to have a chat with a hair transplant expert to find out if it’s the right choice for you.
Core Benefits
- Least invasive of hair restoration solutions
- Quick outpatient process
- No scalpel incision or sutures
- Minimum discomfort
- No linear scar
- Faster recovery time
- Safe and efficient
- Natural results
Is FUE right for me?
Determining if FUE is the right option for you involves considering various factors, and here is a simplified explanation:
Firstly, think about your hair loss pattern. FUE works best for people with certain types of hair loss, usually those who have bald patches but still have a good amount of hair on the back and sides of their head.
Secondly, consider your personal expectations. Do you want a method with minimal scarring and quicker recovery time? If yes, FUE might be suitable for you.
Next, think about your budget. FUE can be quite expensive, especially if you need several sessions. Make sure to consider if you are ready for the financial commitment it requires.
Lastly, it’s important to have a detailed consultation with a hair transplant specialist. They can assess your hair and scalp condition and guide you on the best method for your individual case.
If FUE fits your hair loss pattern, meets your expectations, and suits your budget, it could be the right choice for you. Remember to have a detailed chat with a specialist to make the best decision.
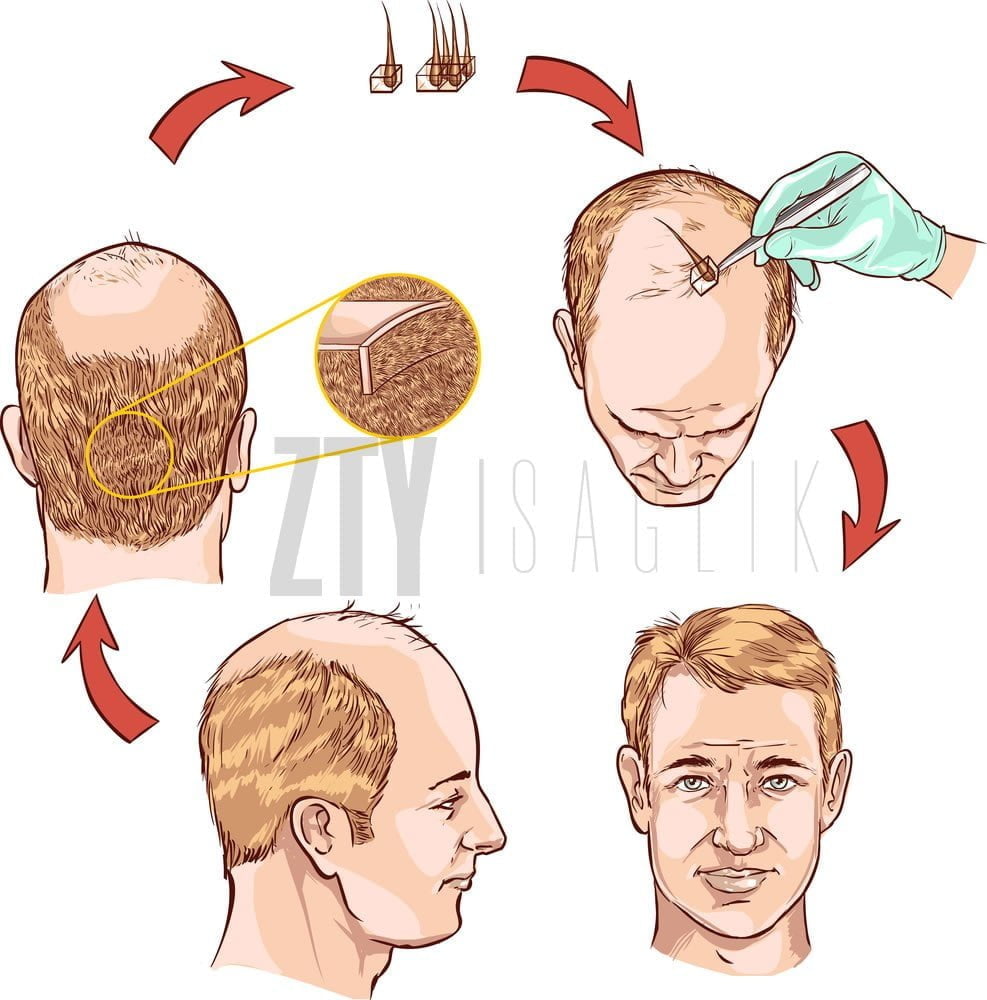
How FUE works
The FUE hair transplant process works in a few clear steps, and here’s a straightforward explanation:
First, the surgeon shaves the donor area, usually the back or sides of your head. Then, using a special tool, they remove individual hair follicles from this area. These are tiny units of 1 to 4 hairs. Next, the surgeon makes tiny holes in the scalp where the hair will go. This is the area where you have thinning or balding. The removed hair follicles are then placed into these holes. Since the follicles are taken one by one, it leaves no noticeable scars and tends to heal fast. This method also allows for a very natural-looking result, as the surgeon can place the hairs with a lot of precision.
After the procedure, you’ll need some time to recover. The new hairs will grow in over the next several months. It might take some time, but the goal is to have a fuller, natural-looking head of hair in the end. Before you decide on this procedure, talk with a specialist to see if it’s the best option for you.
What Are The Risks Of Fue Hair Transplant ?
Follicular Unit Extraction (FUE) hair transplant is generally considered a safe procedure, but like any surgical procedure, it comes with potential risks and complications. Here are some of the most common risks associated with FUE hair transplantation:
- Infection and Scarring: While FUE hair transplantation is minimally invasive and typically results in less visible scarring than other methods, there’s still a risk of infection and scarring.
- Bleeding: Some bleeding is common during and after the procedure, but in rare cases, excessive bleeding can occur.
- Swelling and Pain: Some degree of pain and swelling is to be expected after surgery, especially in the first few days. These are generally manageable with over-the-counter pain medications and should resolve on their own.
- Numbness or lack of sensation: Some patients report a temporary loss of sensation in the treated areas. This usually resolves over time.
- Unnatural Appearance: If the procedure is not done properly, the transplanted hair may appear unnatural. This is more a risk related to the skill of the surgeon than the procedure itself.
- Poor Hair Growth: Not all the transplanted hair follicles will necessarily survive and grow hair. This may result in uneven hair growth or less density than anticipated.
- Folliculitis: After a hair transplant, patients may experience inflammation or infection of the hair follicles, known as folliculitis. This is typically a short-term issue and can be treated with antibiotics or compresses.
- Shock Loss: This refers to temporary hair loss in the areas surrounding the transplant. This usually recovers over time, but in rare cases, it may be permanent.
- Psychological Impact: The recovery process can take several months and the final result may not be apparent for up to a year. Some patients may experience anxiety or disappointment during this period.
Post-Hair Transplant Recovery and Growth Timeline
| Timeframe | Healing Process and Clinical Observations | Hair Growth Status |
|---|---|---|
| First 24-72 Hours | Mild pain, edema (swelling), and erythema (redness) may be observed in the donor and recipient areas. Swelling can extend to the forehead and periorbital region. Elevation of the head is recommended. | Grafts begin to anchor in the recipient sites. |
| Week 1 (Days 3-10) | Formation of scabs or crusts occurs at the recipient sites. The initial hair wash is performed at the clinic. Pruritus (itching) is a normal sign of wound healing. The scabs typically begin to shed between days 7 and 10. | No discernible new hair growth is expected at this stage. |
| Weeks 2-4 | Most scabs have exfoliated, and erythema has substantially subsided. The onset of “shock loss” (effluvium) is expected; this is a normal physiological process where the transplanted hair shafts are shed. | The transplanted hairs are shed as the follicles enter the telogen (resting) phase. |
| Months 2-3 | The donor and recipient areas are largely healed. The process of shock loss may be complete. Some patients may experience folliculitis, presenting as small, acne-like pustules. | The hair follicles remain in the telogen phase. No significant visible growth occurs. |
| Months 4-6 | New hair shafts begin to emerge from the scalp. Initially, they may be fine, thin (vellus-like), and curly in texture. The growth pattern can be asynchronous and irregular. | The initial phase of new hair growth becomes apparent. Approximately 40-50% of the final result may be visible. |
| Months 7-9 | The hair continues to increase in length and caliber (thickness). There is a noticeable improvement in hair density and scalp coverage. | The rate of hair growth accelerates and becomes more prominent. Approximately 60-70% of the final result can be observed. |
| Months 10-12 | The hair shafts thicken further, lengthen, and acquire their natural texture. The hairline and overall aesthetic appearance are well-established. | Approximately 80-90% of the final outcome is achieved. The hair is now long enough for styling. |
| Months 12-18 | This period represents the final maturation phase. The hair has reached its maximum thickness, density, and has fully matured. | The final result is realized. The transplanted hair appears completely natural and is fully integrated with the native hair. |
Who Should Undergo Fue Hair Transplantation?
Both men and women can opt for Fue hair transplantation. It can be performed in anyone who suffers from hair loss due to genetic factors.
What are the Advantages of Fue Hair Transplant?
- It has a short healing process since Fue hair technique is not a surgical operation.
- There is no scarring as hair is transplanted by opening up micro channels.
- Provides very natural results and leaves behind no marks.
- Causes no pain as it is performed under local anesthesia.
- Does not cause damage to hair follicles.
After fue hair transplant
After your FUE hair transplantation at our hair transplant clinic, it’s necessary to rest at the hotel for a day. The following day, we will escort you back to the clinic for a hair wash. And on the day after that, we’ll take you back to the clinic to have the stitches removed.
RELATED: Dhi Hair Transplant
What role do follicular units and grafts play in hair transplantation
Hair follicles are structures that envelop the hair roots in the form of vesicles and are responsible for anchoring, producing and growing hair. When it comes to the FUE and FUT technique, doctors often speak of follicular units. Medicine understands this to mean hairs that grow so close together that they form a group that belongs together. A follicular unit contains up to five hair roots. In modern hair surgery, the surgeons no longer transplant all the hair individually, but transplant whole follicular units at the same time.
This allows for a much more natural end result. The English word Graft means transplant. In the context of hair transplant, this means all follicular units that are removed from the donor area and reinserted in the recipient area. Doctors differentiate between micro- and minigrafts: the former consist of one to two hairs and the latter three to four.
How Many Sessions Are Required?
Number of sessions for Fue hair transplant depends on how many grafts are required. Duration of each session varies according to the number of grafts that will be transplanted. They averagely last 4 to 6 hours.
What are the Postoperative Instructions?
The donor area should be kept dry in the first three days and no application should be performed other than the solutions given by the doctor. At the end of the third day, the hair should be washed in the clinic and the hair should be washed every day for the next week. In this way, the hair follicles are strengthened. It is necessary to protect the implant area against direct impact during this period.
How Long Does It Take For Hair To Grow After Transplantation?
The hair follicles will completely fall out 3 weeks after the surgery. This is also called shock hair loss. The follicles remain in the transplantation area during this process. The follicles remaning in the waiting phase for 90 days begin to grow back after the shedding process. The hair grows back in patches and the hair restoration is completed within about 8-10 months. hair transplant turkey
Does the Transplanted Hair Fall Out?
The transplanted hairs do not fall out since the follicles are taken from the area which is genetically resistant to hair loss.
Where It is Performed?
The hair transplantation procedure is performed in our clinic in Istanbul.
RELATED: Beard Transplant
FUE Risks
There are common risks associated with all types of surgery. Possible complications are like infection, excess bleeding, unsatisfactory results, and pain. FUE carries some unique risks. The most common are the risk of follicle damage, as each follicular unit I directly extracted from the scalp. When a follicle is damaged, it is unlikely to produce hair when inserted within the scalp. The hairline should be studied well in the FUE technique. To create a natural hairline in the FUE technique is difficult.
What is FUE Technique?
As you know in hair transplantation, hair follicles are extracted from the forehead from the nape area. It is transplanted to the bald area. In the FUE technique, hair follicles are extracted one by one manually from the forehead. This is a painstaking task. These grafts, which are removed one by one, are separated according to their directions. During the planting phase, each hair follicle is dealt with separately by transplanting to the bald area one by one. The FUE technique gives successful results. Labor and art lie beneath this. In hair transplantation with FUE, hair follicles are not taken only from the nape area. If necessary, follicle units can be collected from many parts of the body, including the chest, arms, legs, and back.
Who is a good candidate for FUE?
Every patient prefers the FUE technique because of its high success rate and a scarless method. However, some patients may not be suitable for the FUE technique. FUE is a better fir for patients who:
Having enough hair follicles, have straight and wavy hair texture, have limited scalp elasticity, people who should not have very curly hair, not having excessive hair loss, patients who want to cover wounds or trauma scars. The FUE technique may be preferred in patients to need to get bck to work or resume other duties quickly.
Why Fue Turkey ?
- Having the best fue hair transplant centers in Turkey.
- The costs are very, very low compared to Europe and America.
- Opportunity to visit the historical places of Turkey.
- The use of advanced technologies such as micro fue in Turkey.
- Low cost per graft in Turkey.
- High competition in Fue hair transplant in Turkey. Handcrafted from the highest level.
Our location on the map
FAQ
Last Update: 15.10.2025